The 2024 American Counseling Association (ACA) conference included an eye-opening presentation by Dr. Sylvia Lindinger-Sternart from the University of Providence and Dr. Varinder Kaur from the University of Detroit Mercy on the intersection of trauma and substance use disorder. Their presentation, “Interrelatedness of Trauma and Substance Abuse,” offered a comprehensive dive into how unresolved traumas can leads to substance use disorders (SUD), and how holistic treatment approaches are so crucial in addressing both trauma and substance use disorders, especially in underserved communities.
Understanding the Connection
The link between trauma and substance abuse disorders (SUD) continues to be an area of important study in the mental health and addiction treatment fields. Trauma, or exposure to an incident or series of events that are emotionally disturbing or life-threatening, can have lasting adverse effects on mental health and can lead to adjacent mental health conditions. In many cases, those who experience significant traumas either in childhood or adulthood are diagnosed with Post-Traumatic Stress Disorder (PTSD).
The National Center for PTSD estimates that approximately 6% of Americans are likely to experience trauma-related PTSD at some point in their lives. Substance use disorder, a primary derivative factor of trauma-related PTSD, has seen significant increases over the past 10-years. In 2021, an estimated 46.3 million people in the U.S. battled SUD, according to Substance Abuse and Mental Health Services Administration (SAMHSA).
Ther correlation between trauma-related PTSD diagnosis and SUD is reported by the National Center for PTSD, which reported that 44.6% of individuals diagnosed with PTSD also meet criteria for SUD. This correlation further emphasizes why addressing both trauma-related PTSD and SUD within a dual treatment plan are important to ensuring a more wholistic and sustained recovery. This is especially true when considering the Social Determinants of Health (SDOH) and its impact on the recovery process.
ACA Presentation Focus Points
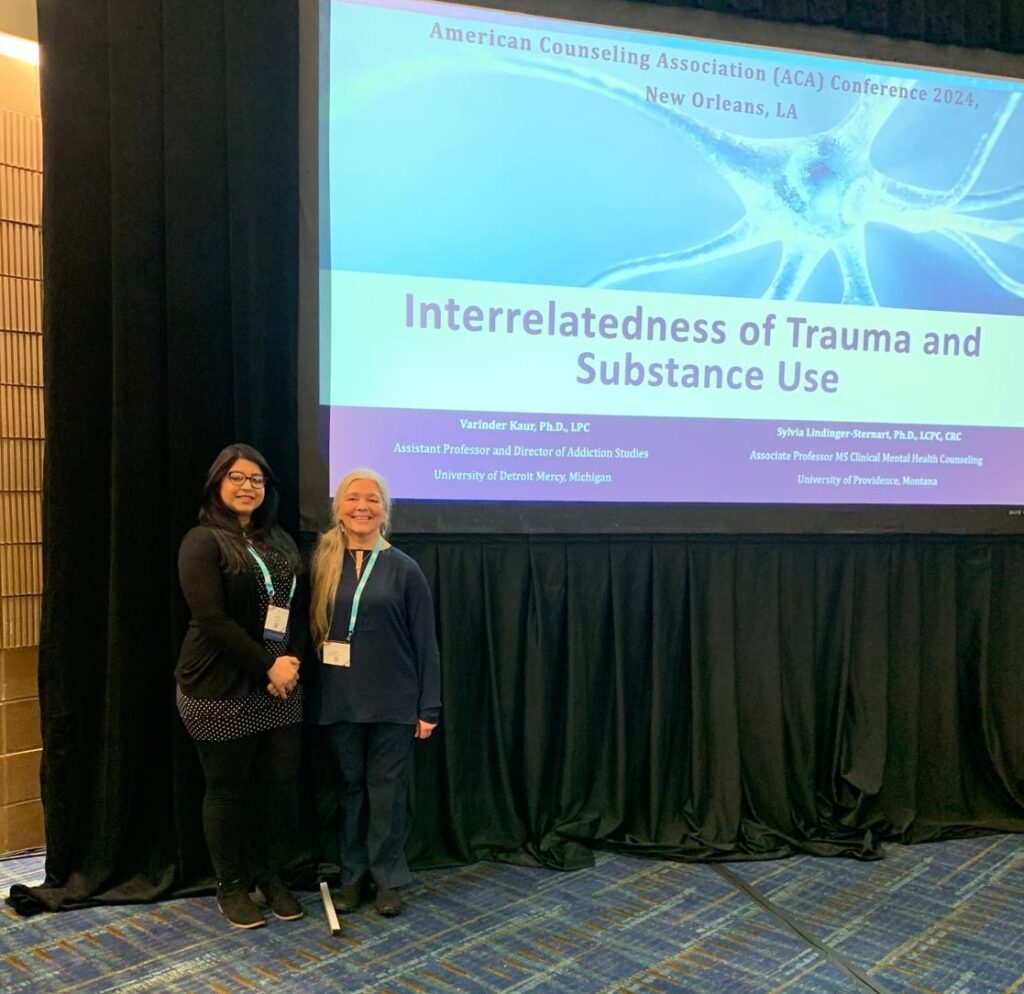
The presentation by Dr. Lindinger-Sternart and Dr. Kaur outlined a wholistic approach to addressing both trauma-related PTSD and substance use disorders “The presentation discussed the underlying reasons of drug abuse, an analysis on the enabling factor, the reinforcing factors of addiction and the synthesizing of the specific role of integrating cultural traditions into professional counseling through the lens of a holistic approach.” said Lindinger-Sternart, who has worked in both clinical and educational capacities with trauma, PTSD, substance abuse, rehabilitation, and holistic healing approaches.
The topics relevance and the importance of its study drew positive feedback from viewers “The audience was very engaged and provided some positive feedback such as expressing the importance of studying the contributing factors of addiction more in depth in underserved populations who use substances often as a kind of self-medication before they get addicted.” said Lindinger-Sternart.
Preparing Counselors Through Education
The education of future clinicians will play an important role in how these diagnoses are treated in tandem with one another. The University of Providence’s Master of Science in Clinical Mental Health Counseling program provides counseling students with a comprehensive understanding of these vital issues through courses offered in both the core Clinical Mental Health Counseling curriculum and in optional concentrations in Addiction Counseling and Clinical Rehabilitation Counseling.
“The program addresses the topic of unresolved trauma and interrelatedness to substance use disorders in the course of how to counsel the addicted client, crisis intervention, and clinical courses,” said Lindinger-Sternart. As research and focus on the subject does, so will the need for a specialized course that focuses exclusively on trauma and its connection to SUD and other mental health problems, like depression, and anxiety.
Looking Ahead
The conversation around trauma and substance abuse will continue to grow as awareness of how traumatic experiences, especially in childhood, impact not just our minds but our bodies too. “Traumatic experiences, particularly adverse childhood experiences, impact not only the psychological health but also physiological systems such as heart variability, immune system, and brain development,” Lindinger-Sternart said. Understanding why people turn to substances as a coping mechanism, an oftentimes generational struggle, will help drive the future emphasis on trauma-informed care and a broader understanding of trauma’s ripple effects on health.
